Chapter 11 Section 3 Tobacco Use Affects the Family and Society
This guidance is issued jointly by the Department of Wellness and Social Intendance, the Welsh Government, the Department of Health Northern Republic of ireland, Public Health England, NHS England and NHS Improvement and with the support of the British Association for the Study of Customs Dentistry.
Delivering Better Oral Health has been developed with the support of the 4 Uk Chief Dental Officers.
Whilst this guidance seeks to ensure a consistent UK wide arroyo to prevention of oral diseases, some differences in operational commitment and organisational responsibilities may utilize in Wales, Northern Ireland and England. In Scotland the guidance will exist used to inform oral health improvement policy.
Smoking in the UK
Smoked tobacco in the course of cigarettes, pipes and cigars, together with all other forms of tobacco, present a major run a risk to oral health. The overall goal of the dental team is to help eliminate all forms of tobacco utilise. It'southward worth highlighting at the showtime that much of the tobacco research has been conducted in relation to cigarette smoking in adults and therefore this may exist reflected in the terminology used, where prove is presented in the summary tables (Chapter ii: Tabular array 3) and in the text beneath.
Despite fewer people smoking, it remains the leading cause of preventable expiry and disease in the Britain (1). Between 2016 and 2018, 77,600 deaths were owing to smoking per year in England with comparable estimates of v,000 deaths each year in Wales, 10,000 in Scotland and 2,300 in Northern Ireland (i). Furthermore, exposure to second-hand fume (passive smoking) can pb to a range of diseases, many of which are fatal, with children especially vulnerable to the effects of passive smoking (2).
Smoking and other forms of tobacco have a meaning affect on ill health and health inequalities. Tobacco use, including both smoked and smokeless tobacco, seriously affects oral health likewise as general wellness. The most meaning risk is for oral cancer and pre-cancer. It is besides the most mutual risk factor for periodontal disease.
In 2019, amongst adults in the UK:
- 14.1% were current smokers (half-dozen.9 million) with the population of England reporting lower levels (13.nine%) compared with Northern Republic of ireland (xv.half-dozen%) Wales (15.5%) and Scotland (15.iv%)
- fifteen.nine% of men smoked compared with 12.v% of women
- younger adults (aged 25 to 34 years) continued to have the highest proportion of electric current smokers (19.0%)
- prevalence was two.v times higher in people in routine and transmission occupations than in people in managerial and professional person occupations: whereas effectually 1 in 4 people (23.2%) in routine and manual occupations smoked, compared with but one in 10 people (10.two%) in managerial and professional occupations
- since 2014, there accept been statistically significant declines in the proportion of current smokers among all socio-economic groups; nevertheless, inequalities have increased
- near people have upward smoking in their teens or early twenties
Source: Part for National Statistics (ONS), 2020.
The prevalence of smoking as well varies within countries, and changes over time so it may be helpful to cheque local rates for your expanse equally listed in the resource at the end of this department.
Smoking rates in people with alcohol and other drug dependencies are 2 to 4 times those of the general population (iv).
Smokers are less likely to report having very expert health (3), when compared with those who have never smoked (1, five); reporting bad or very bad general health was more than than 2.v times as common in current smokers than those who accept never smoked (12.two% and 4.7%, respectively) (five).
In Great Britain, more half (52.vii%) of people aged 16 years and to a higher place who currently smoked said they wanted to quit and 62.5% of those who have ever smoked said they had quit (ane). Almost cigarette smokers report that they would like to stop and make many attempts to quit. Currently, around one-half of all smokers quit using willpower lonely (6). However, receiving back up tin can greatly increase a person's chances of quitting successfully.
People are iii times equally probable to quit successfully if they utilise a combination of finish smoking aids (including e-cigarettes) together with specialist assistance and support (six, 7).
Supporting smokers in contact with the healthcare organization to quit is a prevention priority in the NHS Long Term Plan and every wellness care professional person has a role to play (8 to x).
Recent research evidence has focused on interventions during infirmary care. A Cochrane Review by Rigotti and others (11) found that hospital based stop smoking interventions that begin during a hospital stay and include counselling with follow-up back up for at to the lowest degree one calendar month afterwards belch are constructive in increasing quit rates. Such programmes are constructive when administered to all hospitalised smokers, regardless of their reason for admission. Adding nicotine replacement therapy (NRT) to a counselling programme increases the success rate of a programme for hospitalised smokers (11). Infirmary based programmes that include behavioural support, pharmacotherapy and follow-upwards have also been shown to reduce all-cause re-admissions and bloodshed at one and ii-year follow-up (12).
Every bit many of the adverse effects of tobacco use on the oral tissues are reversible, stressing their affect on oral health may provide a useful ways of motivating patients to quit. Quitting smoking is the best affair a smoker can practise for their health, and the benefits of stopping begin almost immediately.
The greatest benefits to oral wellness relate to preventing periodontal diseases (Affiliate 5) and oral cancer (Chapter 6). The most significant harms of tobacco use on the mouth are oral cancers and pre-cancers, increased severity and extent of periodontal diseases, tooth loss and poor wound-healing mail service-operatively (13, xiv). Reducing tobacco utilise is a key priority for the NHS across the four nations of the Britain.
Chewing tobacco and other tobacco products
Dental team members should be aware of the various alternative forms of tobacco and alternative forms of utilize such as chewing rather than smoking and that these are associated with oral cancer, other oral pathologies and negative health effects (xv). Information on the use of other tobacco products inside the UK is more than limited than smoking; however, a recent oncology paper highlights that the utilise of smokeless tobacco is becoming a global concern (16). Smokeless tobacco is responsible for a large number of deaths worldwide with the S Eastward Asian region begetting a substantial share of the brunt (17).
The use of betel quid (paan) with areca nut, with or without the addition of smokeless tobacco, is especially mutual within South Asian civilization and oral cavity cancer is very common in the Indian sub-continent (18). Its social and cultural apply is observed beyond the UK (nineteen), with some evidence that it is impacting on the adventure of oral cancer (20, 21).
Shisha smoking (too known as hookah, water pipage, narghile or hubble bubble) is a traditional method of tobacco use, especially in the Eastern Mediterranean region, but its employ is observed across the world. Many people wrongly perceive waterpipe smoking as less harmful than smoking considering of the perception that water filters out the harmful substances in the smoke. Still, it's associated with many of the same risks equally cigarette smoking. Like smoking, shisha smoking produces significant levels of noxious chemicals including tar, carbon monoxide (CO), nitric oxide and diverse carcinogens (22, 23).
Nasal snuff fabricated from pulverised tobacco leaves is a dry grade of tobacco which is inhaled or 'snuffed' into the nasal crenel. Moist snuff typically used in Scandinavia is known equally Snus. Snus can be loose or pre-packaged in small teabag-like sachets. Other countries have different forms of dried or moist tobacco used for sniffing, dipping or chewing (24, 25). Chewed tobacco comes in a number of forms, loose-foliage, dip, plug, twist and chew numberless.
New products are continually emerging such equally 'Heat-not-burn' tobacco products (HnB); these are electronic devices that heat procedure tobacco instead of combusting information technology to supposedly deliver an aerosol with fewer toxicants than in cigarette smoke (26). Bear witness is primarily drawn from tobacco industry information and lacks research on long-term HnB use effects on health (26).
All forms of tobacco that are legal in the Great britain present an oral cancer risk and users of tobacco in any form tin can be helped to quit through smoking cessation interventions (27 to 29). It'south important to enquire people if they use smokeless tobacco, using the names that the various products are known by locally. If necessary, testify them a moving-picture show of what the products look like, using visual aids (28) as shown below (Figure eleven.1), or by using this link.

Figure 11.one: Nicotine tobacco products adapted from Metropolis of Bradford MDC
Common names for products containing tobacco include:
-
waterpipes, shisha, hookah, hubble-bubble (containing tobacco and flavourings)
-
zarda (tobacco often added to paan)
-
gutkha (processed tobacco with added sweeteners)
-
scented chewing tobacco (tobacco with added flavours)
-
naswar, nas, niswar (tobacco with slaked lime, indigo, cardamom, oil, menthol, water)
-
chillam (heated tobacco)
-
paan (tobacco, areca nut or 'supari', slaked lime, betel foliage)
-
snuff, snus (powdered or ground tobacco)
-
khaini (tobacco, slaked lime paste, sometimes areca nut)
This may exist necessary if the person'southward first language does not include English language or if the terms are unfamiliar. Although at that place has been less research on smokeless tobacco use, a similar arroyo to delivering very cursory advice is recommended (Table 2.iii) for patients who are users (30). Advising of the health risks, using the same cursory intervention and referring patients who want to quit to specialist back up services is recommended. The outcome then needs to be recorded in the patient notes, as with all tobacco employ.
Effective interventions to support patients to quit smoking
Healthcare practitioner advice, provided across a diverseness of healthcare settings, helps people stop smoking (31).
Research suggests that 95% of patients look to exist asked about smoking and a short intervention can make all the difference (32). Smokers are more likely to expect to exist asked about tobacco use and recognise the demand to modify than people with other hazard behaviours (33).
Dental teams are in a unique position to provide opportunistic advice to many 'healthy' people who need professional person support to finish their tobacco employ and reduce their risk of oral disease. The commencement phase is to constitute if the patient is a smoker, of any course of tobacco. Dental teams across primary intendance, community and infirmary services routinely investigate tobacco employ every bit office of standard patient care. Communication tin can and so be given most effective methods of quitting smoking involving behavioural and pharmacological approaches as outlined in Figure 11.ii: Very cursory communication pathway: 30 2d discussion.
Very Cursory Advice
Very Brief Communication (VBA) from the dental squad (28, 29, 34), as outlined in the bear witness tables (Chapter 2, Tabular array 3), has been shown to increment a patient'southward motivation to quit and can double a patient's success with quitting smoking (28, 29). Dental professionals tin can successfully deliver tobacco abeyance interventions to increase the chances of achieving long‐term tobacco‐apply abstinence; this includes single and multi‐session behavioural back up, and behavioural support with the addition of NRT or eastward‐cigarettes (29). Many people will, however, need VBA on a number of occasions before they are fix to deed. Keep asking and advising because it volition brand a difference (35).
Ask most smoking
All patients (adolescents and adults) should have their smoking status (electric current smoker, ex-smoker, never smoked) established at the beginning of a form of dental care, recorded, and checked at every opportunity. This is part of a normal medical history routine in a dental setting and should be explored during the consultation.
Do you smoke?
The member of the dental team who elicits this information should ensure this information is recorded in the patient'due south clinical notes.
For those with or at chance of oral affliction, nearly notably oral cancer, pre-cancer or periodontal illness, due to smoking or tobacco utilise, it is of import to give VBA.
Advise on the best way of quitting
Inform patients that the best way of quitting is with a combination of specialist support and medication (36).
Advice involves making a unproblematic statement such equally:
The best way to terminate smoking is with a combination of behavioural support and stop smoking aids, which tin significantly increase the chance of stopping.
Medications that improve the chances of adults quitting smoking include combination nicotine replacement therapy (NRT), varenicline, and bupropion (37 to 40).
E-cigarettes or vapes are not risk complimentary merely are far less harmful than cigarettes and there is growing evidence that they can help smokers to stop smoking (41 to 43).
The traditional approach to advice has been to warn a smoker of the dangers of smoking and advise them to end. This is deliberately left out of VBA for 2 reasons: beginning, it can immediately create a defensive reaction and heighten feet levels and, 2nd, it takes fourth dimension and can generate a conversation about smoking utilize, which is more advisable during a dedicated terminate smoking consultation.
Act according to the patient's motivation
For those who wish to finish, refer to specialist support services where these are available (42). If not available, information technology will be of import to actively refer (not signpost) them to their GP or pharmacist:
Would you like me to refer y'all for specialist terminate-smoking advice and support?
For those who are non ready to stop, assert that this opportunity volition remain open to them with:
That is fine, but help is bachelor. Allow me know if you modify your mind.
A summary of the smoking-pathway, which is useful for all forms of tobacco, is presented in Effigy 11.ii.
Harm reduction
Ceasing smoking reduces damage, ideally stopping permanently, or temporarily for example preceding an operation. Other people may reduce in stages and and then stop. People who are not ready or willing to terminate smoking completely may wish to consider using a nicotine-containing production to help them reduce their smoking en route to harm reduction. Dental team members should familiarise themselves with the Dainty guidance on Smoking: damage reduction (44) and the recommendations in NICE Guidance NG92 (42. Almost all of the harm from smoking is caused by other components in tobacco smoke, non by the nicotine. Smoking is highly addictive, largely because it delivers nicotine very quickly to the brain and this makes stopping smoking hard. Nicotine-containing products are an effective fashion of reducing the harm from tobacco for both the person smoking and those around them. It is less harmful to utilize alternative nicotine-containing products than to smoke (xl).
Local services
Skillful back up from local stop smoking providers, combined with the use of stop smoking aids gives smokers the all-time chance of quitting for good. Depending on the area, services tin be based in a range of settings including integrated lifestyle services, community pharmacies and GP surgeries farther information can exist found on the NHS website.
End smoking back up is free (with the exception of prescription charges where applicative) and offers a selection of one-to-one or grouping behavioural support from a trained stop smoking advisor together with pharmacotherapy. Smokers who receive this packet of support are 3 times every bit probable to quit successfully as those who try to quit unaided or with over the counter NRT.
Dental team members should find out what specialist finish smoking providers (ideally local stop smoking back up) are bachelor locally for their patients. Referral to local providers for back up tin be made quicker and easier by adding a template into your existing data management arrangement.
Where none is available then patients should be directed towards their GP or pharmacist. Furthermore, information technology is helpful to be aware if at that place are specific local programmes such as voucher schemes for pregnant women to stop smoking, given that dental care is free during pregnancy this presents an ideal opportunity to support smoking cessation. A trial conducted in ane centre showed that women in Glasgow were 2.63 times more likely not to be smoking at the stop of pregnancy when incentives were provided for supported smoking cessation (45).
Overview of quitting methods
one. Local stop smoking services
They offer the best chance of success. Combining terminate smoking aids with proficient behavioural support makes someone iii times every bit likely to quit as using willpower lone.
2. Using a stop smoking medicine
A end smoking medicine prescribed past a GP, pharmacist or other health professional person doubles a person's chances of quitting.
iii. Using over-the-counter nicotine replacement
NRT such as patches, gum or e-cigarettes makes it one and a half times every bit likely a person volition succeed.
four. Using willpower lone
This is the least constructive method.
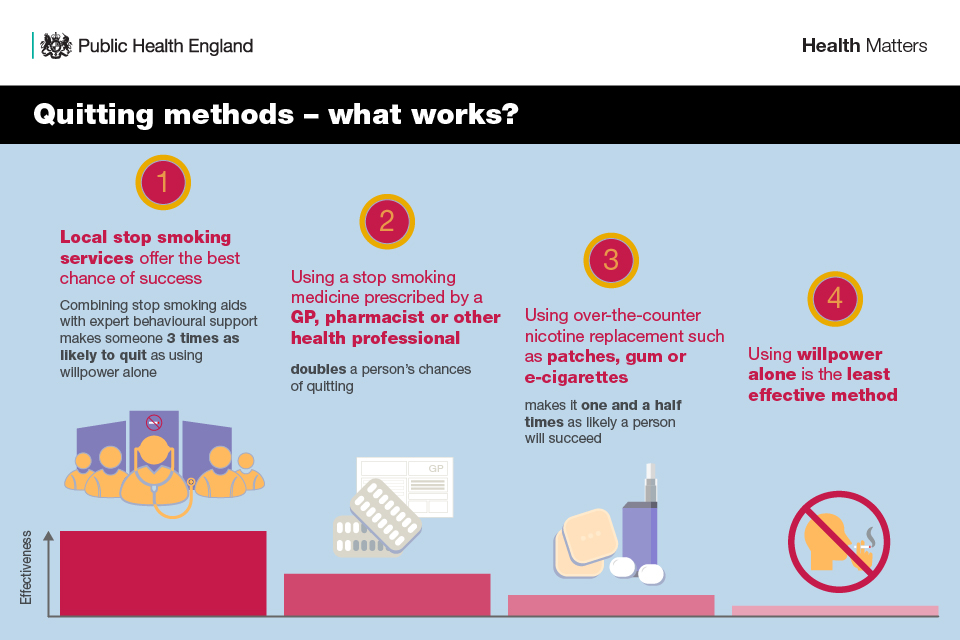
Figure xi.3. Quitting methods
Pharmacotherapy
Pharmacotherapy is particularly constructive when used in conjunction with behavioural support. Many of these products are available over the counter in a pharmacy or other retail outlets.
About of the research involves adults and is related to cigarette smoking. Whilst the dental team may not exist involved in prescribing these products, patients may choose to either obtain them elsewhere on prescription or purchase them. So it is helpful to be aware of the evidence and to heave patients' confidence in using them.
NRT, varenicline and bupropion have all been shown to amend the chances of quitting smoking in adult smokers.
Testify suggests that:
-
combination NRT (a patch combined with a fast-interim product) or varenicline are equally effective as quitting aids (38)
-
all of the licensed forms of NRT (gum, transdermal patch, nasal spray, inhalator and sublingual tablets or lozenges) can help people who brand a quit attempt to increase their chances of successfully stopping smoking. NRTs increase the charge per unit of quitting by 50% to 60%, regardless of setting (46)
-
combination NRT is more than effective with regard to long term quit rates than a single form of NRT in adults who are motivated to quit (39)
-
college dose (21 mg/24-hour) nicotine patches result in college quit rates than lower dose (14 mg/24-60 minutes) nicotine patches in those motivated to finish smoking (39)
-
there is no evidence of a difference between fast-acting NRT, such as gum and lozenge, and nicotine patches in those motivated to stop smoking (based on high quality prove) (39)
-
varenicline may exist more effective than bupropion with regard to quit charge per unit and relapse (37)
-
varenicline improves abstinence compared with bupropion or NRT, however it is more likely than placebo to lead to nausea, indisposition, abnormal dreams, headaches and serious adverse events. The lack of comparative adverse furnishings assessment of varenicline with bupropion or NRT ways that business firm conclusions of the overall comparative effects of these interventions cannot exist drawn (47)
-
NRT may increase the chances of quitting during pregnancy nonetheless, evidence is low certainty (48). In that location is no testify that NRT is harmful in pregnancy and licensed NRT medication is routinely used to aid abeyance
Whilst patients may be prescribed varenicline or bupropion, the drug of choice is nearly likely to exist varenicline unless in that location are medical contra-indications (49). Varenicline reduces cravings for nicotine by blocking the advantage pathway and by reinforcing furnishings of smoking which accept identify in the brain (fifty). Bupropion (Zyban) reduces urges to smoke and helps with withdrawal symptoms (l).
Considering the specific safety concerns, contraindications (for example, bupropion is contraindicated in patients who have seizures), and comorbidities, the choice of agent is based largely on patient preference afterwards discussion with a clinician (49). Current evidence suggests that adverse events for these interventions are mild and would not mitigate their use, although concerns accept been raised that varenicline may slightly increase cardiovascular events in people already at increased run a risk of these illnesses (37, 38).
There is a growing body of evidence evidence that behavioural interventions combined with nicotine replacement, provided by dental professionals, may increase tobacco forbearance rates in cigarette smokers (29).
Clinical trials have largely been conducted among adults; thus, in children, there is no evidence to support the employ of pharmacological interventions (51). NRT is licensed for use in children over 12 years of age in the Great britain.
Reducing smoking
If a patient indicates involvement in cut downwards their smoking, the healthcare professional person should inform them that health benefits come from stopping smoking altogether. Any benefits of simply reducing are unclear.
However, the clinician should advise them that if they reduce their smoking at present, they are more probable to stop smoking in the time to come, particularly if they use licensed nicotine-containing products to help reduce the amount they smoke (40).
People who reduce the amount they smoke without supplementing their nicotine intake with a licensed nicotine product tend to compensate by drawing smoke deeper into their lungs, exhaling later and taking more than puffs. Therefore, use of a licensed nicotine-containing product to provide 'therapeutic' nicotine is recommended.
Alongside the strong safety profile of NRT, the benefits of advising smokers unwilling or unable to quit smoking to reduce their smoking using NRT are likely to outweigh any disadvantages, given that the culling is likely to be no action (40).
The Stoptober campaign during the calendar month of October provides an opportunity for smokers to quit, as people who stop smoking for 28 days are 5 times more probable to quit for skillful (52).
Safety of nicotine: evidence and misconceptions
While nicotine is the addictive substance in cigarettes, it is relatively harmless (9).
In fact, about all of the harm from smoking comes from the thousands of other chemicals in tobacco fume, many of which are toxic.
Despite this, research finds that amidst smokers and ex-smokers in the United kingdom (22):
- only vi in ten think that NRT is less harmful than smoking cigarettes
- just 4 in 10 incorrectly think nicotine in cigarettes causes most of the smoking-related cancer
Given these misconceptions, advising smokers on the relative safety of nicotine containing products compared to smoked tobacco is an integral role of supporting them to quit.
People should exist advised to use NRT, or an eastward-cigarette if they choose every bit it will help them to manage their cravings when they stop smoking.
Vaping (e-cigarettes)
Due east-cigarettes, also known as vapes, are the most popular stop smoking aid in England, with 2.5m users in 2019 (9, 53).
There are many unlike types of east-cigarette product and this market is quickly changing.
E-cigarettes are electronic devices that heat a liquid, usually containing nicotine, to create an droplets for inhalation. At present, at that place is no medicinally licensed e-cigarette product bachelor on the United kingdom of great britain and northern ireland market place. Nonetheless, the UK has some of the strictest regulation for e-cigarettes in the globe. Under the Tobacco and Related Products Regulations 2016 (54), e-cigarette products are subject to minimum standards of quality and safety, likewise as packaging and labelling requirements to provide consumers with the data they need to make informed choices.
All e-cigarette products must be notified past manufacturers to the Britain Medicines and Healthcare products Regulatory Agency (MHRA), with detailed information including the listing of all ingredients. Leading Great britain health and public wellness organisations including the Royal Higher of General Do, British Medical Association and Cancer Research Great britain now agree that although non gamble-costless, e-cigarettes are far less harmful than smoking (l).
Only a very small proportion of young people, who have never smoked, report that they vape (<one%) (55). More than half of current vapers have managed to stop smoking completely and it is estimated that e-cigarettes may help over l,000 smokers a year in England to quit smoking, who would non have done then by other means (56).
E-cigarettes are particularly constructive when combined with a structured programme of behavioural support. A major Great britain clinical trial found that, when combined with practiced face-to-face support, people who used e-cigarettes to quit were twice as probable to succeed than people who used other nicotine replacement products such as patches or gum (57). People who have completely switched to vaping should be recorded every bit not-smokers in dental records.
NICE guidance NG92 (42) sets out the following recommendations for health and social intendance workers in primary and community settings.
For people who smoke and who are using, or are interested in using, a nicotine-containing due east‑cigarette on full general sale to quit smoking, explain that:
-
although these products are non licensed medicines, they are regulated past the Tobacco and Related Products Regulations 2016 (54)
-
many people have constitute them helpful to quit smoking cigarettes
-
people using e‑cigarettes should stop smoking tobacco completely, because any smoking is harmful
-
the testify suggests that e‑cigarettes are substantially less harmful to wellness than smoking only are not risk complimentary
-
the evidence on e-cigarettes is still developing, including prove on their long-term health impact
In summary, in that location is growing evidence that due east-cigarettes are helping many thousands of smokers in England to quit. The available show from inquiry trials suggests that their effectiveness is broadly like to prescribed stop smoking medicines and meliorate than NRT products if these are used without whatever professional back up. Eastward-cigarettes are specially effective when combined with expert aid from a local finish smoking service.
Implementation and delivery in dental practice
The National Centre for Smoking Abeyance and Preparation (NCSCT) has adult a simple form of advice designed to exist used opportunistically in less than a minute in almost any consultation with a smoker.
All dental team members should exist encouraged to undertake the NCSCT grooming as part of regular continuing professional development, therefore ensuring all dental squad members are competent to deliver VBA and brief interventions in smoking cessation.
The most common intervention dental teams volition be involved in is delivering Enquire, ADVISE, Deed in line with VBA to smokers (Figure 11.2). Use of the evidence-informed pathway will increase the chance of a successful quit attempt. It just takes thirty seconds and tin requite patients the motivation to proceeds professional aid which volition increment their chances of quitting. It is important to be aware of policies, services and routes of access in your local healthcare system equally these vary across the UK. A like arroyo can exist followed with all tobacco users.
The best outcomes occur when those who are interested in stopping take-up a referral for specialist support. Timing is crucially important: the quicker the contact past a local stop smoking service, the greater the motivation and involvement from the individual. Dental patients who express a desire to end should exist referred to their local specialist stop smoking support (ideally a local stop smoking service) to receive the best opportunity to stop smoking.
Dental teams and the local stop smoking services can work collaboratively in a diversity of means. Every bit a first pace, information technology's important that all members of a dental team are fully aware of the services offered locally and of how these operate. Arranging a coming together with a representative of a local provider could provide a useful opportunity for dental teams to learn nearly the service offer and the best ways of referring dental patients.
Information technology'south important that no matter who makes the referral, the patient's progress in stopping is assessed and is recorded in their clinical notes at each subsequent dental appointment.
Stopping tobacco use tin be a difficult procedure and is oftentimes associated with a range of unpleasant, short-term withdrawal symptoms, some of which, such as ulcers, direct affect the rima oris.
Reassurance and advice from dental team members may help patients deal more effectively with these issues, thereby increasing their chances of quitting successfully.
The Cochrane review on tobacco cessation interventions (58) provided during substance abuse handling or recovery is particularly helpful in managing patients who may have more than one addiction. Current testify suggest that providing tobacco cessation interventions targeted to smokers in handling and recovery for booze and other drug dependencies increases tobacco abstinence.
Resources
NCSCT Very Brief Advice on Smoking for Dental Patients.
eastward-Learning for healthcare: Booze and Tobacco Cursory Interventions program.
NHS – Quit Smoking.
Find your Local Stop Smoking Service (LSSS).
Smoking and tobacco: applying All Our Health.
Wellness matters: stopping smoking – what works?.
Stop smoking options: guidance for conversations with patients.
Due east-Cigarettes policy, regulation and guidance.
ASH: Activity on Smoking and Health (ASH) is a public health charity that works to eliminate the harm acquired by tobacco.
Local Tobacco Control Profiles.
The example for delivering Very Brief Advice on smoking YouTube video:
YouTube video
References
1. Office of National Statistics. Developed smoking habits in the UK: 2019. London: ONS; 2020 7 July 2020.
2. Center for Disease Control. Health Effects of Secondhand Smoke. CDC; 2020 [updated 27 Feb 2020].
3. NHS Digital. Statistics on Women'south Smoking Status at Time of Delivery, England – Quarter 3, 2017 to 2018](https://digital.nhs.uk/data-and-data/publications/statistical/statistics-on-women-due south-smoking-status-at-time-of-delivery-england/statistics-on-women-s-smoking-status-at-time-of-commitment-england-quarter-3-2017-18). NHS Digital UK; 2018 [updated ten May 2018].
iv. Kalman D, Morissette SB, George TP. Co‐morbidity of smoking in patients with psychiatric and substance use disorders. American Journal on Addictions 2005;14:106‐
5. ONS. Adult smoking habits in the United kingdom of great britain and northern ireland: 2018. London: Office for National Statistics; 2 July 2019.
6. Public Health England. Health matters: stopping smoking – what works? London: PHE; 17 December 2019.
seven. NHS. Quit smoking.
8. NHS England. NHS Long Term Plan. London: NHS England; 2019 [updated 7 Jan 2019].
ix. UK Authorities. E-cigarettes and heated tobacco products: show review. In: Care DoHaS, editor. [edited 2 March 2018] London: Great britain Government; 2018.
x. Nice. Making every contact count. London: National Institute for Health and Clinical Excellence; 2021 [24 Apr 2021].
eleven. Rigotti NA, Clair C, Munafò MR, Stead LF. Interventions for smoking cessation in hospitalised patients. Cochrane Database of Systematic Reviews. 2012(5).
12. Mullen KA, Manuel DG, Hawken SJ, Pipage AL, Coyle D, Hobler LA and others. Effectiveness of a hospital-initiated smoking cessation programme: ii-year wellness and healthcare outcomes. Tobacco Control. 2017;26(3):293-ix.
thirteen. Johnson NW, Bain CA. Tobacco and oral disease. British Dental Journal. 2000;189(4):200-vi.
xiv. Hashibe M, Brennan P, Chuang SC, Boccia S, Castellsague X, Chen C and others. Interaction betwixt tobacco and booze use and the risk of head and cervix cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2009;eighteen(2):541-50.
fifteen. Gupta B, Johnson NW. Systematic review and meta-assay of association of smokeless tobacco and of betel quid without tobacco with incidence of oral cancer in South asia and the Pacific. PloS one. 2014;9(eleven):e113385.
16. Mehrotra R, Yadav A, Sinha DN, Parascandola G, John RM, Ayo-Yusuf O and others. Smokeless tobacco control in 180 countries across the world: call to action for full implementation of WHO FCTC measures. The Lancet Oncology. 2019;20(4):e208-e17.
17. Sinha DN, Suliankatchi RA, Gupta PC, Thamarangsi T, Agarwal N, Parascandola M and others. Global brunt of all-crusade and cause-specific bloodshed due to smokeless tobacco use: systematic review and meta-analysis. Tobacco control. 2018;27(1):35-42.
xviii. Gupta PC, Arora M, Sinha D, Asma S, Parascondola M. Smokeless Tobacco and Public Health in India. Ministry building of Health and Family Welfare, Government of India; 2016.
nineteen. Panesar SS, Gatrad R, Sheikh A. Smokeless tobacco employ by southward Asian youth in the UK. The Lancet. 2008;372(9633):97-8.
20. Csikar J, Aravani A, Godson J, 24-hour interval M, Wilkinson J. Incidence of oral cancer among S Asians and those of other ethnic groups by sex in West Yorkshire and England, 2001–2006. British Journal of Oral and Maxillofacial Surgery. 2013;51(1):25-9.
21. Tataru D, Mak V, Simo R, Davies EA, Gallagher JE. Trends in the epidemiology of caput and neck cancer in London. Clinical Otolaryngology. 2017;42(1):104-xiv.
22. Wilson Southward, Partos T, McNeill A, Brose LS. Damage perceptions of east‐cigarettes and other nicotine products in a Uk sample. Addiction. 2019;114(five):879-88.
23. Perraud V, Lawler MJ, Malecha KT, Johnson RM, Herman DA, Staimer N and others. Chemical label of nanoparticles and volatiles present in mainstream hookah fume. Aerosol Scientific discipline and Technology. 2019;53(9):1023-39.
24. FDA. Smokeless Tobacco Products, Including Dip, Snuff, Snus, and Chewing Tobacco. Silverish Leap, MD: Usa Nutrient & Drug Administration; 2020 [updated 23 June 2020].
25. Earth Wellness Organization IAfRoC. Smokeless Tobacco and Some Tobacco-specific N-Nitrosamines. Lyon, France: WHO IARC; 2007.
26. Simonavicius E, McNeill A, Shahab L, Brose LS. Rut-not-fire tobacco products: a systematic literature review. Tobacco control. 2019;28(5):582.
27. Maziak W., Jawad 1000., Jawad Due south., Ward K.D., Eissenberg T., Asfar T. Interventions for waterpipe smoking abeyance. Cochrane Database of Systematic Reviews 2015(seven).
28. Carr AB, Ebbert J. Interventions for tobacco abeyance in the dental setting. Cochrane Database of Systematic Reviews. 2012(6).
29. Holliday R, Hong B, McColl E, Livingstone-Banks J, Preshaw PM. Interventions for tobacco cessation delivered past dental professionals. Cochrane Database of Systematic Reviews. 2021(ii).
30. Prissy. Smokeless tobacco: South Asian communities. Public Health Guideline [PH39]. London: Dainty; 2012 02.x.2010. Contract Number: PH39.
31. Stead LF, Perera R, Bullen C, Mant D, Hartmann-Boyce J, Cahill K and others. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2012;eleven:Cd000146.
32. Slama KJ, Redman S, Cockburn J, Sanson-Fisher RW. Community Views About the Role of Full general Practitioners in Affliction Prevention. 1989;six(3):203-9.
33. Brotons C, Bulc G, Sammut MR, Sheehan Thou, Manuel da Silva Martins C, Björkelund C and others. Attitudes toward preventive services and lifestyle: the views of primary intendance patients in Europe. The EUROPREVIEW patient study. Family Practice. 2012;29 (supplement ane):i168-i76.
34. Aveyard P, Begh R, Parsons A, Due west R. Brief opportunistic smoking cessation interventions: a systematic review and meta-analysis to compare advice to quit and offer of assistance. Addiction (Abingdon, England). 2012;107(6):1066-73.
35. NHS England, Health Teaching England, Public Health England. Alcohol and Tobacco Cursory Interventions Programme: NHS England; 2019.
36. Stead LF, Koilpillai P, Fanshawe TR, Lancaster T. Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Database of Systematic Reviews. 2016(3).
37. Cahill K, Lindson‐Hawley N, Thomas KH, Fanshawe TR, Lancaster T. Nicotine receptor fractional agonists for smoking abeyance. Cochrane Database of Systematic Reviews. 2016(5).
38. Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta‐analysis. Cochrane Database of Systematic Reviews. 2013(v).
39. Lindson N, Chepkin SC, Ye W, Fanshawe TR, Bullen C, Hartmann‐Boyce J. Different doses, durations and modes of commitment of nicotine replacement therapy for smoking abeyance. Cochrane Database of Systematic Reviews. 2019(iv).
40. Lindson‐Hawley N, Hartmann‐Boyce J, Fanshawe TR, Begh R, Farley A, Lancaster T. Interventions to reduce harm from continued tobacco apply. Cochrane Database of Systematic Reviews. 2016(x).
41. Flach S, Maniam P, Manickavasagam J. E-cigarettes and head and cervix cancers: A systematic review of the current literature. Clinical otolaryngology: official journal of ENT UK. 2019;30.
42. Dainty. Terminate smoking interventions and services [NG92]. London: Nice; 2018 28.03.2018. Contract No.: NG92.
43. Hartmann‐Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Database of Systematic Reviews. 2016(9).
44. Prissy. Smoking: harm reduction PH45. London: National Institute of Clinical Excellence; July 2013.
45. Tappin D, Bauld Fifty, Purves D, Boyd K, Sinclair Fifty, MacAskill S and others. Financial incentives for smoking cessation in pregnancy: randomised controlled trial. British Medical Journal. 2015;350:h134.
46. Hartmann‐Boyce J, Chepkin SC, Ye W, Bullen C, Lancaster T. Nicotine replacement therapy versus control for smoking abeyance. Cochrane Database of Systematic Reviews. 2018(v).
47. Bunt C. How does varenicline compare with bupropion or nicotine‐replacement therapy for smoking cessation? Cochrane Clinical Answers. 2017.
48. Claire R, Chamberlain C, Davey MA, Cooper SE, Berlin I, Leonardi‐Bee J and others. Pharmacological interventions for promoting smoking cessation during pregnancy. Cochrane Database of Systematic Reviews. 2020(three).
49. Rigotti Northward. Pharmacotherapy for smoking cessation in adults 2020 [updated 27 Feb 2020].
50. United kingdom Government. Smoking and tobacco: applying All Our Health. London: United kingdom of great britain and northern ireland Government; 2020 [updated 16 June 2020].
51. Fanshawe TR, Halliwell Westward, Lindson North, Aveyard P, Livingstone‐Banks J, Hartmann‐Boyce J. Tobacco cessation interventions for young people. Cochrane Database of Systematic Reviews. 2017(xi).
52. NHS. STOPTOBER: quit smoking with Stoptober. London: NHS; 2019 [updated iii Apr 2018].
53. McNeill A., Brose L., Calder R., Bauld L, Robson D. Vaping in England: an bear witness update including mental wellness and pregnancy, March 2020. London: Public Wellness England; 2020.
54. HM Regime. The Tobacco and Related Products Regulations 2016. London: Public Health England,; 2016. Contract Number: SI507.
55. McNeill A, Brose L, Calder R, Bauld L, Robson D. Vaping in England: an show update February 2019. London: Public Health England; 2019.
56. Beard E, W R, Michie Southward, Brown J. Association of prevalence of electronic cigarette use with smoking abeyance and cigarette consumption in England: a time–serial assay between 2006 and 2017. Habit. 2020;115(5):961-74.
57. Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N and others. A Randomized Trial of E-Cigarettes versus Nicotine-Replacement Therapy. New England Journal of Medicine. 2019;380(7):629-37.
58. Apollonio D, Philipps R, Bero L. Interventions for tobacco utilize cessation in people in treatment for or recovery from substance apply disorders. Cochrane Database of Systematic Reviews. 2016(11).
thomasonvorcy1981.blogspot.com
Source: https://www.gov.uk/government/publications/delivering-better-oral-health-an-evidence-based-toolkit-for-prevention/chapter-11-smoking-and-tobacco-use
0 Response to "Chapter 11 Section 3 Tobacco Use Affects the Family and Society"
Post a Comment